Countries in the WHO European Region commit to applying behavioral and cultural insights when developing health policies, services and communications
On September 13, health ministers representing over 900 million people in the WHO European Region have agreed to use Behavioral and Cultural Insights (BCI) to better inform the successful development, implementation and evaluation of health-related policies, services and communications.
The adoption of the BCI Action Framework took place at the 72nd session of the WHO Regional Committee for Europe, WHO’s annual governance meeting for the European Region, in Tel Aviv, Israel.
Advancing Behavioral and Cultural Insights is a flagship initiative of the WHO European Program of Work, and a BCI Unit was established by WHO/Europe in 2020 to lead efforts and provide technical guidance to countries.
“How we improve health goes far beyond providing better medical care,” said Dr Hans Henri P. Kluge, WHO Regional Director for Europe. “We have long known that structural, individual and cultural factors – such as convenience, clear messaging, financial incentives, social norms and support, religion, and family – have a strong influence on the effectiveness of policies to enhance people’s health. But, until now, such factors have not been explored extensively or applied systematically.
How we improve health goes far beyond providing better medical care
“The action framework on behavioral and cultural insights that countries have committed to implement is the first of its kind, and will keep the European Region at the forefront of this innovative and promising field. It will ensure that these invaluable, evidence-informed insights receive the attention and investment they deserve, and feed into health policies, services and other interventions to help people lead happier, healthier lives,” he added.
Developed through a broad one-year consultative process with nationally-nominated focal points and other experts, the action framework outlines five strategic commitments where countries should take action. They will report on their progress over its 5-year timeframe from 2022-2027.
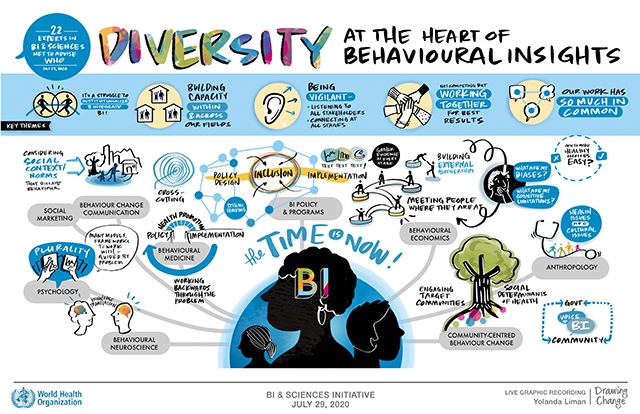
These commitments are to engage stakeholders; conduct research to explore the barriers and drivers people face in leading healthy lives; include this insight in the design of health-related policy, services and communications; invest in sustainable BCI capacity; and develop national plans to implement BCI.
Many proven examples exist of applying BCI.
Convenience, clear messaging, financial incentives, social norms and support, religion, and family have a strong influence on the effectiveness of policies to enhance people’s health
• France consulted with food manufacturers and retailers, scientists and consumers to design effective front-of-pack-labelling with clear nutritional information, to positively influence consumer food purchases, and the ‘Nutri-Score’ was adopted in 2017.
• In 2016, the Government of the United Kingdom announced that a soft drinks industry levy would come into effect in 2018. Its design and implementation were informed by a public consultation in 2016.
Acknowledging that individual behavior change is challenging, the tax targets producer behavior by encouraging reformulation, as the tax escalates according to sugar levels in the drink. As a result, the soft drinks industry has significantly reduced the amount of sugar in their products, leading to a 30% reduction in sugar sold per capita per day from soft drinks.
• Patients with tuberculosis in the Republic of Moldova were more likely to keep to their treatment program when it was made more convenient – with health care professionals observing adherence through video connection, rather than in-person. On average, TB patients missed only 1.29 days of treatment with this new approach, compared to 5.24 days, over a two-week period.
• Doctors in the United Kingdom who had previously been identified as high prescribers of antibiotics, reduced their prescriptions by 3.3% over a 6-month period after receiving a letter from the country’s chief medical officer indicating that they prescribed more than most other medical practices in their local area.
Why use BCI?
Research indicates that individual behavior and social circumstances together account for 60% of factors determining people’s health.
BCI work means investigating and understanding the structural, individual and cultural factors that affect health behaviors, and using these insights to improve the results of health-related policies, services and communications.
It can be used to define problems, conduct research into root causes, understand barriers and drivers of health behaviors, inform program planning and implementation, as well as to test and evaluate which interventions work. This evidence-based discipline builds on existing work and methodologies from diverse fields including psychology, sociology, economics, anthropology, political science and cultural studies.
Further information
European regional action framework for behavioral and cultural insights for health, 2022–2027
https://apps.who.int/iris/handle/10665/360898
Draft resolution: European regional action framework for behavioral and cultural insights for health, 2022–2027
https://apps.who.int/iris/handle/10665/361521
Case examples of applying BCI to health-related policies, services and communications processes
https://apps.who.int/iris/handle/10665/361653